In this teaching scenario, consultant Bill discusses the importance of early detection when treating familial hypercholesterolaemia
A healthcare professional talks about his experience of treating patients with familial hypercholesterolaemia: a relatively common, dominantly inherited genetic condition. Bill also explains the positive impact of early detection on effective treatment and management.
Read Bill’s story below and use the teaching moments and discussion points to design your teaching session.
AT-A-GLANCE
Clinical focus: Cardiology, common conditions
Nursing activities: Identification, management and ongoing care, communication, family care, education
NMC platform and outcomes: 1 (1.8, 1.9, 1.13, 1.18); 2 (2.2, 2.4, 2.5, 2.9, 2.10); 3 (3.1, 3.2, 3.5, 3.11, 3.12, 3.15, 3.16); 4 (4.2, 4.3, 4.5, 4.15); 5 (5.4); 7 (7.1, 7.8)
Bill’s story
Identification and diagnosis
1 I work with lipid disorders but particularly with familial hypercholesterolaemia (FH), a dominantly inherited condition. My job has two parts: I’m a consultant in the clinic where we look after people with these conditions, and I’m also responsible for the laboratories that do a lot of the testing on the blood of these patients.
2 The main test that’s done is cholesterol testing and the different reaction to cholesterol. The test can measure total cholesterol, low-density cholesterol and high-density cholesterol. In patients with FH, those levels are high. For many of these tests, a period of fasting is required – usually between 12 and 24 hours. This type of testing is a requirement for diagnosis, alongside other indicators such as family history of sudden cardiac death or high cholesterol in the young.
3 Although cholesterol testing is standard, a genetic test is also well established and is being rolled out across the UK. The genetic test can look for genes we know to be responsible for FH. Genetic and genomic testing is developing all the time and, as we have been testing for FH for a significant length of time, we have a good knowledge of the molecular test and genetic variants involved in FH.
Treatment and management
4 FH is very amenable to treatment if diagnosed at the right time. Our understanding is better than it once was, as are the treatments – in particular, the cholesterol-lowering tablets. We’ve now got very good evidence that if you can treat the LDL cholesterol in these individuals, the risk of coronary disease will be reduced. I can think of many patients who have been successfully treated and their cholesterol levels have come down, their coronary disease has been treated with cardiac procedures, angioplasty, and they are leading healthy normal lives, whereas otherwise they would have been debilitated by heart failure and other complications of cardiovascular disease.
5 The importance of getting the right treatment at the right time is highlighted in the following example. We have a patient who attends our clinic: a lady in her fifties who had coronary artery bypass grafts when she was younger – and she knew that her son had also inherited the condition. Unfortunately, her son had been lost to follow-up and had not really appreciated the significance or the benefits of the treatment. As a result of our efforts to improve the follow-up for patients and families with FH, the mother had contacted her son again and made it clear that it was important. From this, he contacted our specialist nurse who suggested that he got his cholesterol checked and get back in touch. He did have his cholesterol checked, but sadly his mother phoned two days later to say that he had died – he was only in his early forties. This was an entirely preventable occurrence, and it makes us realise that if we had better referral systems in place or better treatments available when this man was in his thirties, this wouldn’t have happened. There are numerous examples like this, particularly in younger men because they are at higher risk.
Raising awareness
6 FH has an incidence of about 1-in-250 of the general population, which is high for a genetic condition, yet it is still under-recognised and underappreciated. There are lots of reasons why. It’s often silent until it causes problems. Raised cholesterol, to some extent, is quite common, and people tend not to treat it with the significance that it deserves. Until recently, treatments were not as good, and so people didn’t take high cholesterol levels as seriously because they felt that not much could be done about it. Also, it tends to fall between professional areas, so that could be another reason why it has been underdiagnosed in the past.
Specialist services
7 Over the last decade, many more health professionals have been employed to identify, test and, in some cases, manage patients with FH. There is a network of services across the UK that share information to aid and facilitate better family testing. There is still a need for better information, both for healthcare professionals outside these services and the patients and families in their care, though; people don’t know enough about it or understand it.
8 FH nurses are now established in many areas and part of what they do is to educate other health professionals in primary and secondary care about FH diagnosis, referral pathways and testing. I also think other nurses need to be aware, though. For example, cardiac rehab nurses see lots of patients with cardiac disease and some of those patients will have FH, particularly the younger patients who are often not recognised by the doctors and nurses. If rehab nurses are aware of this condition, then appropriate action could be taken. Earlier identification is key.
9 I think there also needs to be an awareness in practice nurses. The relative commonness of the condition means there is every chance that people with FH will be regularly seen by GPs. I think the initial assessment of these patients probably needs to be done in a specialised clinic, but thereafter the management can be followed up in general practice once the patient and those looking after the patient are up to speed with care plans.
The role of nurses
10 Nurses do have a major potential role in this condition: for education, counselling, cascade testing, detection and for advice. Often patients will find it easier to contact a nurse to discuss issues that are concerning them rather than make an appointment to see the doctor. And there are lots of issues that an informed nurse can really help with.
11 In regards to the multidisciplinary team, there a number of different professional groups, but I think there is also a wider disciplinary approach. Within the clinic, there are some general nurses who look after the running of the clinic, then there’s the doctors. Dieticians are important in treating lipid disorders, including FH. Specialist nurses are important for counselling, cascade testing, specialist information and obviously the admin and clerical support within the clinic.
Supporting families
12 As FH is familial, we will often see multiple individuals from the same family, which can be interesting because not all families get on. It does sometimes raise issues. Quite often, you get a parent and an older daughter or son who come to the clinic together and you see them both. That’s not uncommon. Usually what happens is that the parent has developed coronary disease at an early age and, as a result, the children have been tested. Those sorts of families are usually very motivated to look for and receive the treatment. So that is quite often the family unit that you get together. But sometimes you have families where some people in the family just don’t want to know.
13 The most important aspect is awareness raising about FH because early detection really does have huge benefits. This applies for both healthcare professionals and patients. I think there could be a role here for expert patients. It’s a condition where people can learn enough about it to be able to educate other people.
Educator touchpoints
Teaching moments
Paragraph 1 | What is meant by a dominantly inherited condition?
Paragraph 2 | What is a family history and why are they important?
Paragraph 3 | What genetic tests exist that can look at more than one gene?
Paragraph 10 | What is meant by cascade testing?
Discussion points
Paragraph 2 | Consider common clinical indicators or red flags when identifying genetic conditions, for example, family history, early onset of condition, symptoms in young.
Paragraph 5 | Even though the condition is genetic, it can be managed. How does this challenge the misconception that there’s nothing that can be done about genetic conditions?
Paragraph 7 | What are the benefits of having an understanding awareness of this condition?
Paragraph 9 | Given that FH is relatively common for a genetic condition, which clinical setting is best suited to identify affected individuals?
Paragraph 10 | What are the skills that nurses possess that might lead to patients and their families confiding in them more than other healthcare professionals?
Paragraph 12 | It should never be assumed that other family members would want to know more or be involved. Explore why this might be and your role in these discussions.
Further learning
FOUNDATION KNOWLEDGE
A short animation to help explain dominant inheritance patterns
2 minutes
Learn the different ways that genetic conditions can be inherited within a family
30 minutes
Tips and tools for communicating with patients about genomics
30 minutes
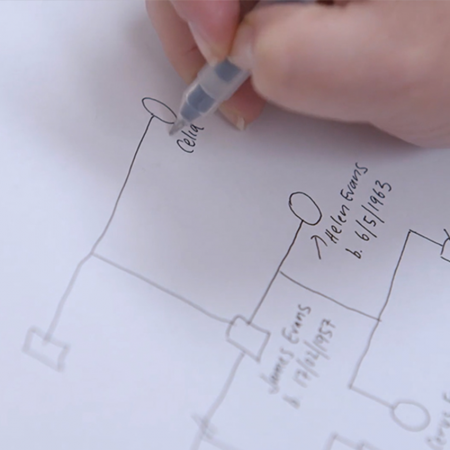
Practical tips and tools to help you read, take and draw a genetic family history
15 minutes
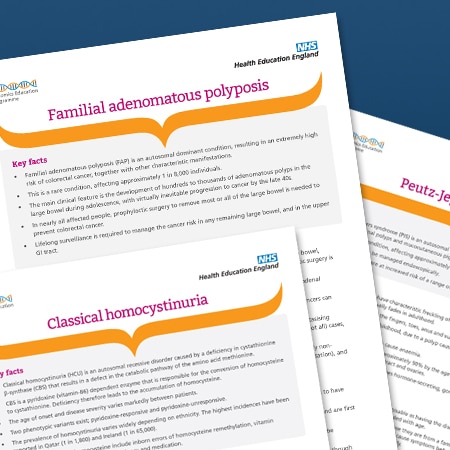
EXTENDED LEARNING
Key facts about the condition, including its clinical features and genetic basis
5 minutes