Cell-free DNA: detecting disease
We look at how cell-free DNA could be used to diagnose LMD – a life-threatening condition that is currently difficult to detect
A recent study has shown the potential of cell-free DNA sequencing to improve detection of a potentially devastating form of metastatic cancer. But how does it work and how could early detection make a difference?
What is cell-free DNA?
Cell-free DNA (cfDNA) are DNA fragments that are found in the blood plasma. They are usually short, double-stranded fragments of between 50 and 200 base pairs, although larger fragments have been observed. These fragments come from cells that die – either from illness or age – as they are broken down by the body.
cfDNA can help us learn more about a person’s own genome. For example, the amount of cfDNA in the blood is a useful biomarker in a range of conditions, including sepsis, diabetes and sickle cell disease. It can also be used to analyse the presence of other genomes, too. Some common uses include non-invasive prenatal testing (the fetus’ genome), and in cancer (the tumour genome).
Leptomeningeal disease
Leptomeningeal disease (LMD) is a possible complication of various types of cancer, where the cancer metastasises to the cerebrospinal fluid. If left untreated, it can significantly reduce survival time to between four and six weeks on average.
LMD can develop after the onset of many different primary cancers, and can affect between 5% and 10% of cancer patients, according to Cancer Research UK. LMD most commonly affects people with breast and lung tumours or melanoma, but can also affect those with other types of solid tumours, as well as blood cancers such as lymphoma and leukaemia.
Diagnosing LMD
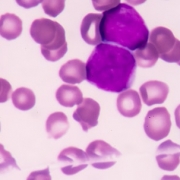
The current methods of diagnosing LMD are not perfect. One available test is cerebrospinal fluid cytologic analysis, where a sample of the fluid that surrounds the brain and spinal cord is taken via lumbar puncture. The cells suspended in the fluid can be separated and tested for the presence of malignant cells.
This test has very high specificity, meaning that false positives are very rare. The false negative rate is high, however – it misses around 25% of cases. Even when the test is repeated multiple times, around 10% of patients return false negatives consistently.
MRI scans are an alternative, but they lack specificity: they can report false positives because other causes can result in a similar appearance to LMD. This can result in over-diagnosis that could cause patients to be subjected to unnecessary treatments and associated side effects.
A new method
Due to the inaccuracy of these existing methods, researchers at Harvard Medical School trialled a new approach that involved looking at cfDNA, rather than whole cells, in the cerebrospinal fluid.
In a small study of 30 patients, they were able to detect LMD in 94% of cases by using genomic sequencing on the cfDNA. There were some false positives in cases where the patient had other tumours close to the cerebrospinal fluid, so cfDNA testing would not be appropriate for these patients. For many, however, this approach could be highly effective – helping more patients receive swift treatment or get enrolled on clinical trials.
The researchers have urged follow-up studies to build on their findings and recommend that prospective trials in LMD include cfDNA analysis.
To find out more about this research, the full article is available to read online.
–