How genome editing could enter mainstream medicine
Forget designer babies and novelty pets. The potential for genome editing to improve the health of the general population is already emerging
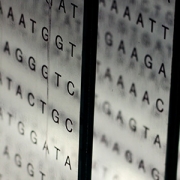
Genome editing – ‘cut and paste’ genetic modification – continues to generate debate, especially on ethical issues related to the potential for making heritable changes to human embryos. Whether to prevent disease or for other forms of ‘enhancement’, the dominance in these discussions of so-called ‘designer babies’ may give a rather skewed view of genome editing and health; such applications would currently be illegal anyway. So what of the less controversial uses of genome editing in medicine?
Back to basics
For the uninitiated, genome editing is simply a set of related techniques that make it possible for any reasonably skilled laboratory scientist to introduce precise genetic changes to a specific section of DNA. Genetic engineering has been around for a long time, but the last few years have seen a rapid change in ease and affordability (and hence accessibility) of the technique.
The main beneficiary has been biomedical research of all kinds. Experiments that would have taken months or years are now much cheaper and quicker. As a result, researchers have scrambled to make use of genome editing for everything from plant science to pig breeding, as well as research aimed at understanding disease and discovering new drugs and treatments.
Medical applications
Genome editing could be used directly for therapeutic purposes, and this is where genetic manipulation of pigs could have a more serious application than breeding novelty pets or even superior farm animals: as a potential source of replacement organs for humans. Xenotransplantation (transplanting organs from one species to another) is fraught with difficulty; finding two humans with a close enough tissue match for a successful transplant is hard enough, without attempting to cross a species barrier. However, genome editing could help efforts to grow human organs inside pigs more safely and effectively – a potential solution to the shortage of donor organs.
Cell-based therapies have already employed genome editing to make customised blood cells to cure patients with severe forms of leukaemia – arguably an ultimate form of personalised medicine – such as in the case of baby Layla Richards. This cleverly combines transplantation of healthy stem cells (in this case to replace leukaemia cells) with genome editing to make those donor cells compatible with the recipient.
Gene therapy in mainstream medicine?
Finally, there is classical gene therapy – introducing ‘corrected’ or healthy genes to replace defective ones that cause disease. While some of the inherent difficulties of gene therapy (getting the healthy genes working reliably in cells in the right part of the body) are not solved by genome editing, it will nevertheless undoubtedly accelerate the development of new therapies.
Most gene therapy trials focus on advanced cancer or severe inherited diseases for which no other treatments are available, but this may not always be the case. One day, gene therapy could be used to combat a much more common medical problem: high cholesterol.
People with genetic mutations that prevent production of the PCSK9 protein have naturally low cholesterol levels, and it has been shown that blocking the PCSK9 protein has a similar effect. Now, AstraZeneca researchers have used genome editing to disable the equivalent gene in mice, leading to speculation that a human gene therapy might be developed to permanently reduce the risk of cardiovascular disease. Such applications are certainly not just around the corner – but they might be closer than we expect.
–