Immortality, regenerative medicine, and the origin of death
Over the past century, huge advances have been made in bioengineering. But what can genomics bring to the table?
With genomics now being used to re-programme cells and assist with the development of new technologies and treatments, be wary of predicting the future, writes Alain Li Wan Po.
Living forever
The Irish playwright and wit George Bernard Shaw once advised us not to try to live forever because we would not succeed. He was perhaps reflecting on the frenetic activity of some of his scientific contemporaries, aimed at understanding and developing methods for achieving cellular immortality and biological rejuvenation: August Weismann, Alexis Carrel, Charles-Edouard Brown-Séquard and Jacques Loeb among others.
Weismann suggested in his essay ‘Theory of continuity of the germplasm’ that death was not inherent in life. The protozoon, he argued, was immortal. When it divides, it leaves no dead body but moves on to form the next generation. He proposed that more complex organisms had merely acquired death as a Darwinian evolutionary trait.
Regeneration and body parts on demand
If immortality were achievable, then being able to replace lost limbs or to regenerate damaged or diseased tissues would be highly desirable. Scientists have addressed puzzles such as why some animals regenerate limbs while the overwhelming majority do not; why our liver (just like that of the Greek god Prometheus) regenerates well but our spinal cord does not; why one fertilised human ovum can lead to so many different types of specialised cells that form the many specialised tissues of the body.
A major step forward was claimed in 1891 when Jacques Loeb, widely regarded as the first biological engineer, reported his success “in finding animals in which it is possible to produce at desire a head in place of a foot at the aboral end, without injuring the vitality of the animal”. While his work generated excitement, applying hydroid bio-engineering to higher animals produced little success. If regeneration was not possible, perhaps rejuvenation might help; Charles Edouard Brown-Séquard conjured up his rejuvenative ‘Elixir of Life’ from animal testicular extracts. His reported success is now attributed to a placebo effect, although testosterone is still widely used to rejuvenate both sex life and young (cheating) athletes.
Experiments in rejuvenation and transplantation
To understand rejuvenative capacity, the leading biologists of the 19th century lopped the tails and limbs off various animals. Worms, another favourite object of study, were shown to regenerate when cut into segments. Such studies – also used to investigate environmental influences on the inheritance of physical traits (Lamarckian versus Darwinian inheritance) – provided no immediate practical benefit.
However, Alexis Carrel (who won the Nobel Prize in 1912) was able to culture fibroblasts from embryonic chicken hearts for considerable lengths of time, and succeeded in maintaining isolated organs alive using a perfusion pump designed by his collaborator, Charles Lindbergh of aviation fame. Improvement in methodology, better understanding of the basis of immunity, and the discovery of immunosuppressant drugs over the following decades eventually led to routinely successful organ transplantation.
Stem cells and cellular therapy
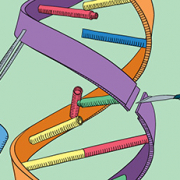
In his 1893 masterpiece, Weismann suggested that there were fundamentally two types of cells in the body: the germ-cells (stem cells) in the reproductive glands, and the somatic cells, which form all other organs and the body itself. The term stem cell now also refers to other cells further along the development path that have the ability to self-renew.
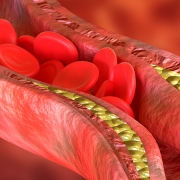
If stem cells, the source of all other cells, regenerate themselves then it should be possible to generate all other cells. This was demonstrated in 1957 with the first successful treatment of a patient with end-stage leukaemia, where doctors used total body irradiation followed by a bone-marrow transplant to kill off the patient’s haematopoietic cells and replace them with healthy ones; an approach which has been progressively improved since then, with better conditioning and careful immuno-matching, to become an important option for the care of patients with an increasing range of diseases.
The work of the early pioneers contributed to the successful use of cultured cells and biodegradable scaffolds to produce engineered tissues for body repairs, as first reported in 2001. Almost a decade later, the first graft was still functional. As a result, cardiologists and surgeons have joined the haemato-oncologists in predicting a bright future for cellular therapy.
Induced stem cells and control of genomic expression
With increasing genomic insights, it has become possible to reprogramme somatic cells to pluripotency, and then to direct their development into other specific cell types (for example, from fibroblast to induced pluripotent cell and thence to cardiomyocyte); initially by direct alteration of the genome but now also with cocktails of small molecules to control transcription and no direct DNA modification.
Moreover, this has been done not only via a pluripotent cell but also directly (fibroblasts to neurons). The enormous implications of this proof-of-principle, not only for cell engineering but also for understanding how our genome interacts with the environment, have yet to be fully appreciated.
With genomics opening up the possibility of such nuanced understanding, and rapid technological advances such as the gene editing technology we recently explored, we should perhaps avoid making a mistake similar to Lord Rutherford’s when he declared that harnessing atomic energy was moonshine; only a few years before this was achieved, and despite the fact that he laid much of the foundation for it. In genomic medicine, what change can come very quickly.
Professor Alain Li Wan Po in editor-in-chief of the Journal of Clinical Pharmacy and Therapeutics, and is a fellow of the Royal Pharmaceutical Society and the Royal Statistical Society.
–