Making sense of mitochondrial disease
The UK has approved new techniques to fix problems in mitochondrial DNA. Here’s how ‘three-person IVF’ will work
The House of Lords has voted in favour of changes to the law to permit the use of new techniques called mitochondrial transfer – also dubbed ‘three-person’ IVF. A majority of MPs in the House of Commons approved the legislative change earlier this month.
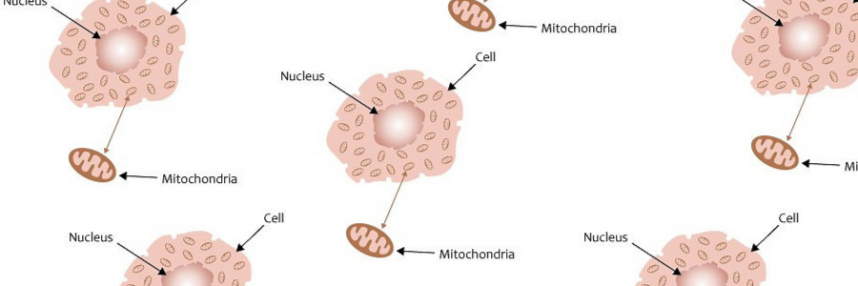
Mitochondria are essential structures that generate most of the energy in living cells. They also contain a small amount of their own DNA – mitochondrial or mtDNA – separate from the rest of the genome in the cell’s nucleus. Most mitochondrial genes are in the nuclear DNA, but the rest are mtDNA.
Where there is DNA, there can be disease, and mitochondrial DNA is no exception. Mitochondrial diseases arise from harmful mutations in mitochondrial genes, both in nuclear and mtDNA. Since the mitochondria are essential, abnormal or inadequate function can have catastrophic effects on multiple body tissues. The time of onset and symptoms can vary widely, but severe forms of mitochondrial disease become symptomatic in infancy and childhood and progress rapidly to death.
Changing the DNA
Researchers have been working for years on techniques to avoid the transmission of diseased mtDNA by women to their children. Because embryos arise at fertilisation from the fusion of egg and sperm cells, egg cells with diseased mtDNA give rise to embryos that have the same diseased mtDNA. The only way to avoid this is to use healthy donor egg cells for in vitro fertilisation (IVF).
Different ways have been developed to remove the donor egg nucleus and replace it with the maternal nucleus either before or just after fertilisation; these techniques are called maternal spindle transfer and pronuclear transfer, respectively. This is why there are, strictly speaking, three biological parents: the father, the mother and the female egg donor. However, the vast majority of DNA comes from the mother and father; only mtDNA from the egg donor is passed on to the resulting embryo, about 0.1% of the total.
Although the donor mtDNA accounts for only a tiny proportion of the embryo’s genome, it is highly significant in a number of ways. First, it is hoped that it will prove sufficient to prevent mitochondrial inherited disease in a resulting child. Secondly, female children would be able to pass that mtDNA on to their own children, so the genetic manipulation, whilst very slight, is a heritable one. And thirdly, for that very reason, it has been illegal.
Changing the law
The amendments to the 2008 Human Fertilisation and Embryology Act exempt the techniques from the blanket prohibition against the modification of nuclear or mitochondrial DNA in human reproductive cells or embryos, where they are to prevent serious mitochondrial disease.
This is no brave new world of unbridled genetic manipulation, though; mitochondrial diseases affect around 1 in 6,500 people, but mitochondrial transfer would only be suitable for a small proportion of at risk couples. Permission to use the technique will also have to be given on a case-by-case basis by the regulator, the Human Fertilisation and Embryology Authority (HFEA) – but this may happen for the first time as early as this year.
Updated on 25 February 2015 to reflect House of Lords decision.
–