‘Omic’ insights into Parkinson’s disease
Recent research reveals potential dawn of personalised medicine for neurological disorders might be more than just ‘gut feeling’
Parkinson’s disease is a neurological disorder that usually develops in people over 50 and leads to progressive deterioration in motor control and cognitive function.
A combination of interacting genetic and environmental factors is thought to be responsible for most cases. In around 15 percent of patients, there is a family history of the disease. This has has been linked to mutations in the LRRK2, PARK2, PARK7, PINK1 and SNCA genes, which may also have role in sporadic cases. These mutations result in nerve cell damage that affects the brain’s ability to produce dopamine, a chemical critical in the control of movement. It is the reduction in dopamine that causes the hallmark symptoms of Parkinson’s such as tremor and muscle rigidity.
Improving drug treatment options
One treatment that has been around for a while is levodopa, which works well in the earliest stages of Parkinson’s but rapidly decreases in effectiveness as the disease progresses. Early stage clinical trials by a US company suggest that MRI-scan guided, surgically delivered gene therapy may allow the drug to be used more effectively in later stages of the disease. Escalating doses of the enzyme aromatic L-amino acid decarboxylase (AADC) reportedly produced increased responses to levodopa in Parkinson’s patients.
Cognitive impairment and emotional disorders are common in people with Parkinson’s, and a new report suggests that mutations in the GBA gene may have a direct link to cognitive decline. Individuals with two defective copies of the GBA gene develop Gaucher’s disease, an inherited metabolic disorder that in its most severe form can cause severe neurological symptoms and death in infancy. People with only one defective copy of the GBA gene are carriers for Gaucher’s, and it has also recently been identified as a common risk factor for developing Parkinson’s disease.
In a study of over 2,000 Parkinson’s patients, around 10% had GBA gene defects and were shown to be at increased risk of memory loss. In the 1-2% of patients with the most severe type of defect, the risk of cognitive decline was more than doubled. Since treatments for Gaucher’s disease are available, these findings have prompted further trials into personalised treatment approaches and new candidate drugs for Parkinson’s.
Gut instinct?
Perhaps most startling among recent research is the suggestion that the gut microbiome may be crucial in Parkinson’s disease. The microbiome is all the genetic material contained within a person’s microbiota, the vast collection of micro-organisms that live in and on the human body. Although the functions of the micro-organisms are shared across all humans, as with the genome, every microbiome is unique.
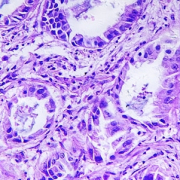
Investigating the gut microbiota in mice genetically programmed to have Parkinson’s, researchers uncovered a link to with motor impairment. Only mice with the gut bacteria developed these symptoms; depletion of the microbiome with antibiotics reduced symptoms, whilst recolonization with fresh bacteria restored them. Moreover, transplanting gut bacteria from human Parkinson’s patients increased the symptoms compared with the effect of using gut bacteria from healthy humans.
Whilst the role of the gut microbiome in Parkinson’s disease has yet to be demonstrated in humans, there is of course great interest in whether the digestive system might hold the key to more effective treatment of Parkinson’s. However, the very characteristics of the microbiome that hold promise for more personalised medicine also make realising this potential a massive challenge.
–