Introduction
Rapid advances in the field of genomics are affecting nearly all areas of healthcare. Nowadays, it isn’t just specialist nurses who are and will be dealing with genomics; all nurses need to have an understanding of where genomics is relevant to their role, which is why genomics is now included in the NMC standards of proficiency for registered nurses. Genomics is increasingly important, and the move towards the NHS Genomic Medicine Service (GMS) will not be possible without the work of nurses across the health service.
Watch this video to learn more about some of the ways in which genomics is used in nursing. The information below expands on the importance of genomics in nursing today, as well as some of the opportunities for nurses in this area.
What do I need to know?
What is genomics?
As nurses, the term ‘genomics’ might seem unfamiliar, but in reality nurses are vital to the delivery of genomic medicine and are already contributing to incredible advances in treatment and care.
Like genetics, genomics also looks at DNA, but improved technology means we can now read all of the information in a person’s or organism’s DNA at once, and in some cases use it to build a clearer picture of health and disease. This is leading to changes in the way we diagnose, treat and care for our patients and their families.
To learn more about genomics, you might like to explore our Bitesize genomics collection.
Why is genomics important in nursing?
There are already many applications for genomics in nursing, with more emerging all the time. Some examples are outlined below.
Family history and early screening
Many people have a family history of a condition – for example, breast cancer or cystic fibrosis. In some of these cases, screening and/or genomic testing can be offered to family members who may have an increased chance of developing a condition. As early screening can save lives and allow early intervention, it is vital that anyone who may benefit is referred for genomic testing. The number of conditions and cancers for which testing and screening are offered is growing all the time. Your patients may be eligible for testing now or next year when they weren’t previously.
Trying to find answers for patients and families
There are around 7,000 rare diseases and many of these are undiagnosed. Undiagnosed rare disease usually affect children, although there are also adults who are yet to receive a diagnosis. Advances are being made in this area all the time, and a new technology known as next-generation sequencing now allows us to sequence the whole human genome (a process known as whole genome sequencing) much more cheaply and quickly than ever before. Increasing numbers of people will be eligible for testing through the new GMS, with the aim of finding answers for more patients.
New advances in common conditions
It isn’t just rare diseases that are benefiting from advances in genomics. Increasingly, genomic testing is being used to better diagnose and/or sub-type common conditions, too. One example of this is monogenic diabetes, which is diagnosed by genomic test and for which a different form of treatment and management is used.
Targeted treatment
Genomic data – that is, information about the DNA of a person or organism – can sometimes enable us to target treatment. For example, many patients receive cancer treatment that is targeted to the genetic mutations within the DNA of their tumour cells, while other medications target the specific DNA mutations of a bacteria – for example, in some cases of TB. In other instances, the genetics of a person themselves can be analysed to see how (and if) they will respond to medication before it is given. This is known as pharmacogenomics and is an area of growth in healthcare.
Research
In order for the great advances that have been made in genomic technology to truly benefit our patients, we need to continue to find new links between genes and disease. There are many opportunities for nurses to be part of research or simply to refer patients who may be eligible for particular research projects. Ultimately, it’s all of our responsibility to take part in the genomics revolution.
How can I play my part?
As you’ve seen in our film, nurses have a unique opportunity to contribute to an effective Genomic Medicine Service. The expectation is not that nurses become experts in genomics (though there are increasingly opportunities to specialise), but there are some key areas where you can really make a difference.
Listen: You may become aware of a medical family history that should be explored, or perhaps an adverse reaction to a certain medication that could be due to genetics.
Observe: Do you know how to spot the signs of genetic conditions in your area of work – for example, developmental delay in children, or a history of a particular disease within a family?
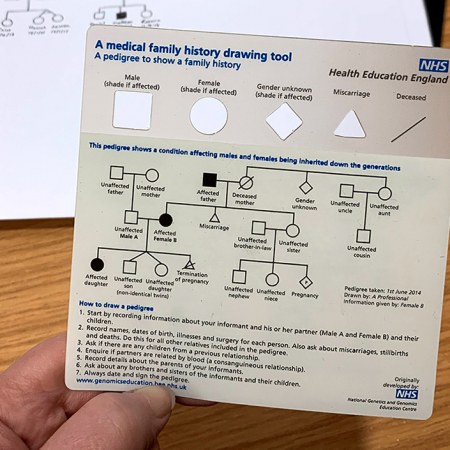
Know how to take a genetic family history:This is often the first step in helping a patient who may benefit from genomic investigations. Our family history collection might be useful to you.
Understand referral options and who to go to/where to go for advice. The most important thing is that we get as many people who could benefit from genomic investigations referred to the right place so that they can benefit from it. Do you know who to contact if you suspect a patient might have a rare genetic condition?
Think genomics: Does your patient have an unusual test result with no obvious explanation? Do you feel that their symptoms don’t quite fit with their primary diagnosis? Both of these could mean that your patient should be referred for genomic testing.
Learn more about genomics and how it’s used – particularly in your area of nursing. Familiarise yourself with the different types of testing so that you can confidently talk to your patients and their family members about genomics and help them understand the process. For example, what sample might be taken for analysis? What might the test mean for them in terms of altering their treatment or management? And what might it mean for their family members?
Roles for nurses
While all nurses will encounter genomics at some point in their practice, there are particular roles where genomics is highly relevant. As new applications for genomics are developed, the number of these roles is likely to increase.
Rare disease
Rare disease nurses support families affected by rare conditions and help them through the health and social care system. Roles in rare disease are often charity funded. For example, Cambridge Rare Disease Network has rare disease nurses, and Birmingham’s Women’s and Children’s Rare Disease Centre has two specialist rare disease nurses funded by Roald Dahl’s Marvellous Children’s Charity.
There are also nurses who specialise in a particular rare condition, such as:
- Familial hypercholesterolemia: These roles usually involve identifying and supporting affected families. You can read more about this work in the North East and Cumbria and the West Midlands.
- Monogenic diabetes: Specialist genetic diabetes nurses support patients with this rare form of diabetes and their families, as well as increase recognition and diagnosis of monogenic diabetes among healthcare professionals. More information can be found here.
Clinical nurse specialist / Advanced nurse practitioner
Nurses working as experts within a particular clinical area, for example oncology, cardiology or ohthalmology, will increasingly be trained in the specific management of inherited genetic conditions and targeted treatment within their area. Keeping abreast of rapid developments in genomics is a key part of the role in many specialisms. Here is an example of the work that a clinical nurse specialist may do, taken from the field of renal medicine.
As new initiatives are developed, it is often appropriate for specialist nurses to become involved with service development to help meet patient needs and address patient demands, with the overall aim of improving patient outcomes. The contact that specialist nurses have with patients means they are uniquely placed to take part in such work.
Research
Although advances in genomics have been rapid and impressive, we still have a long way to go. Ongoing research is vital if we are to ensure that all patients can benefit. There are many opportunities to be involved with research projects as a nurse, and you may choose to specialise in this area. The work may involve developing hypotheses, recruiting patients to research projects, training other members of staff, collecting and analysing data, and caring for and communicating with those patients who are involved.
Board representation
Nurses are valued members on many boards and in collaborations between different organisations and charities. You can hear from Dr Christine Patch about her work with the Global Genomics Nursing Alliance and how to get involved in our podcast.
Learning opportunities
Teaching aids
Clinical resources
Identifying patients
Activity: Taking and drawing a genetic family history
Equip yourself with the knowledge and skills to construct a genetic pedigree.
Activity: Recognising the clinical clues of a genetic condition
Familiarise yourself with the clinical features of a range of genetic conditions
Communicating with patients
Activity: Returning genomic test results to patients
There are a range of factors to consider when returning genomic results to patients, based on whether there is a confirmed diagnosis, an uncertain result or a negative result.
Clinical management
Activity: Support decision-making in a consultation
Equip yourself with the knowledge of a range of genetic conditions and the genomic tests available.
Activity: Signpost your patients to further support
Patient groups and charities can offer vital support and guidance for patients, both pre-and post-diagnosis.