Amniocentesis
Amniocentesis is a clinical procedure performed during pregnancy. It is used to obtain a sample of amniotic fluid from the amniotic cavity.
Indications
Amniocentesis may be performed for the following indications:
- antenatal genomic diagnostic testing;
- fetal structural anomaly;
- higher-chance aneuploidy screening result;
- previous pregnancy affected by a chromosomal genetic condition;
- family history of certain genetic conditions;
- suspicion of certain infections during pregnancy; and/or
- to reduce amniotic fluid quantity in pregnancies with severe polyhydramnios (this is called an amnioreduction).
Procedure
- Amniocentesis is performed after 15 weeks’ gestation. Before this point, there is insufficient amniotic fluid surrounding the fetus to perform the test.
- A detailed ultrasound scan is performed to assess fetal viability, fetal lie, position and placental location.
- The abdomen is cleaned with an antiseptic solution and a pocket (pool) of amniotic fluid is identified.
- Under ultrasound guidance, a fine sterile needle is inserted through the mother’s lower abdomen, the uterus and fused membranes (amnion and chorion) and into the pocket of amniotic fluid.
- A syringe inserted into the top of the needle hub is used to siphon a small amount (about 20 millilitres) of amniotic fluid (again, under ultrasound guidance). The needle is slowly withdrawn from the sample path.
- Fetal wellbeing is assessed with ultrasound to check again for fetal viability following the procedure. The pregnant woman is reassured.
- Use of local anaesthetic is not routinely required.
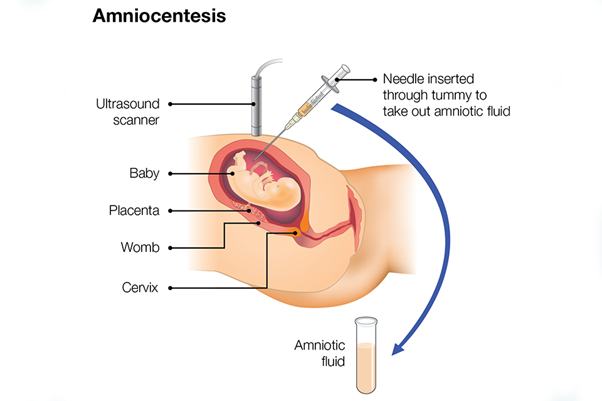
Figure 1: The amniocentesis procedure
Diagram from Gov.uk guidance: Screening in pregnancy: CVS and amniocentesis information for parents. Licensed under the Open Government Licence v3.0.
Risks of amniocentesis
There are certain risks associated with amniocentesis. Some of them are listed below.
- Miscarriage: the chance of miscarriage following amniocentesis is estimated at around 1 to 2 per 200 tests performed (or 0.5%–1%) for a singleton pregnancy. The chance is higher in twin or multiple-order pregnancies, at around 1 per 50 tests performed (or 2%).
- Where amniocentesis is performed later in pregnancy, it may result in iatrogenic preterm labour.
- Infection: the rate of severe infection for amniocentesis is lower than 1-in-1,000.
Other considerations
Patients tend not to describe amniocentesis as painful, but they do usually describe it as uncomfortable.
Amniocentesis is usually very straightforward, but it can be a technically difficult procedure in cases where there is an anterior placenta, or where the amnion and chorion are not fused in their entirety.
It is critical that pre-procedure counselling includes a discussion about the risks discussed above, in order to enable the pregnant woman to make an informed decision about whether to proceed.
Alternative testing may include chorionic villus sampling or non-invasive prenatal testing (this may include non-invasive prenatal screening or non-invasive prenatal diagnosis.
Rhesus status
Maternal rhesus status must be confirmed prior to amniocentesis so that anti-D immunoglobulin can be given to those patients who are rhesus D negative.
Resources
For clinicians
- Royal College of Obstetricians and Gynaecologists: Amniocentesis and chorionic villus sampling (Green-top Guideline No. 8)
References:
- Ghi T, Sotiriadis A, Calda P and others. ‘ISUOG Practice Guidelines: invasive procedures for prenatal diagnosis‘. Ultrasound in Obstetrics & Gynaecology 2016: volume 48, pages 256–268. DOI: 10.1002/uog.15945
For patients
- Antenatal Results and Choices: Amniocentesis
- NHS: Amniocentesis