Hypoplastic left heart syndrome
Hypoplastic left heart syndrome is a congenital condition in which the left side of the heart is underdeveloped. Most cases are of unknown cause, although some genomic variants are being highlighted within research.
Overview
Hypoplastic left heart syndrome occurs when the left side of the heart is underdeveloped: the mitral and/or aortic valve is narrow or blocked, the left ventricle is underdeveloped, the aorta is small and underdeveloped and there is an atrial septal anomaly.
Figure 1 shows the anatomical variance that occurs.
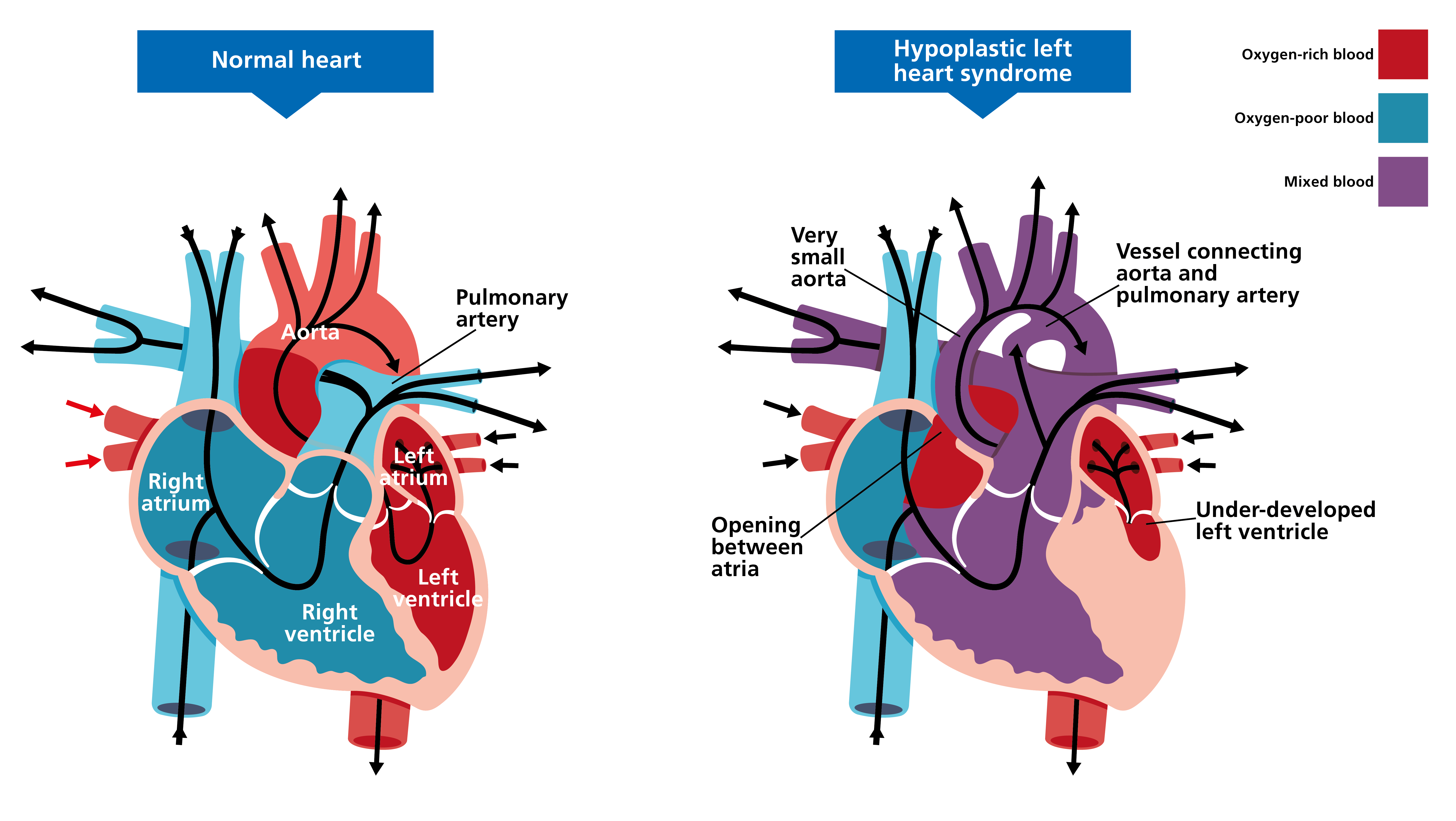
Figure 1: Hypoplastic left heart syndrome
Clinical features
The clinical features of hypoplastic left heart syndrome are:
- dyspnoea;
- a high-pitched noise during inhalation;
- cyanosis;
- congestive heart failure early in life;
- poor feeding;
- frequent vomiting;
- lethargy; and
- life-threatening complications such as shock and hepatomegaly, which can occur if the condition is left untreated.
The progression and severity of hypoplastic left heart syndrome depends on whether the ductus arteriosus remains patent. The ductus arteriosus allows blood to pass from the right ventricle to the aorta, bypassing the left side of the heart. It normally closes soon after birth, but initial treatment in babies with hypoplastic left heart syndrome involves keeping it open until corrective surgical measures can be completed.
Genomics
While in most children with hypoplastic left heart syndrome the cause is not known, there are some cases with genomic findings noted in research settings – for example, variants in NOTCH1 and MYH6.
Occasionally, hypoplastic left heart syndrome is associated with a diagnosis of Turner syndrome, Noonan syndrome or one of the common trisomies (21, 18 and 13).
Diagnosis
Hypoplastic left heart syndrome is commonly detected on prenatal ultrasound and fetal echocardiogram, or it may present clinically at birth.
Characteristic features on echocardiography are:
- hypoplasia of the left ventricle and aorta;
- stenotic or atretic aortic and mitral valves;
- small or hypoplastic left atrium; and
- dilated right ventricle with dilatation of the pulmonary artery trunk.
Chromosomal testing, in the form of common aneuploidy testing (QF-PCR) and microarray, may be considered for some congenital heart conditions. For more information, see Infant or child with congenital heart disease.
Inheritance and genomic counselling
There may be a slightly increased chance of hypoplastic left heart syndrome recurring in a family. The recurrence risk and inheritance pattern may become clearer in those rare cases in which a genomic cause is identified.
The common trisomies and Turner syndrome have around a 1% chance of recurrence.
If a heritable cause of hypoplastic left heart syndrome is suspected, families should be offered genomic counselling to explore their options.
Management
Prostaglandin E1 is given to maintain the patency of the ductus arteriosus before it closes in early life. This allows blood to bypass the problematic left side of the heart.
For the surgical correction of hypoplastic left heart syndrome, there is a three-stage process. This involves a Norwood procedure and a hemi-Fontan procedure, followed by a Fontan procedure. The aim is to separate the systemic and pulmonary circulation.
Occasionally, a heart transplant is the recommended treatment for infants.
Genomic counselling is recommended for families with affected children where there is a known genomic cause.
Resources
For clinicians
- NHS England: National Genomic Test Directory
References:
- Theis JL and Olson TM. ‘Whole genome sequencing in hypoplastic left heart syndrome‘. Journal of Cardiovascular Development and Disease 2022: volume 9, issue 4, page 117. DOI: 10.3390/jcdd9040117
- Yagi H, Liu X, Gabriel GC and others. ‘The genetic landscape of hypoplastic left heart syndrome‘. Pediatric Cardiology 2018: volume 39, pages 1069-1081. DOI: 10.1007/s00246-018-1861-4
For patients
- British Heart Foundation: Understanding your child’s heart: Hypoplastic left heart (PDF, 23 pages)
- Great Ormond Street Hospital for Children NHS Foundation Trust: Hypoplastic left heart syndrome