Diagnostic odyssey in rare disease
The ‘diagnostic odyssey’ is a term used to describe the long and difficult journey that many rare disease patients and their families undertake to receive an accurate diagnosis – a journey that takes, on average, 5.6 years.
What is the diagnostic odyssey?
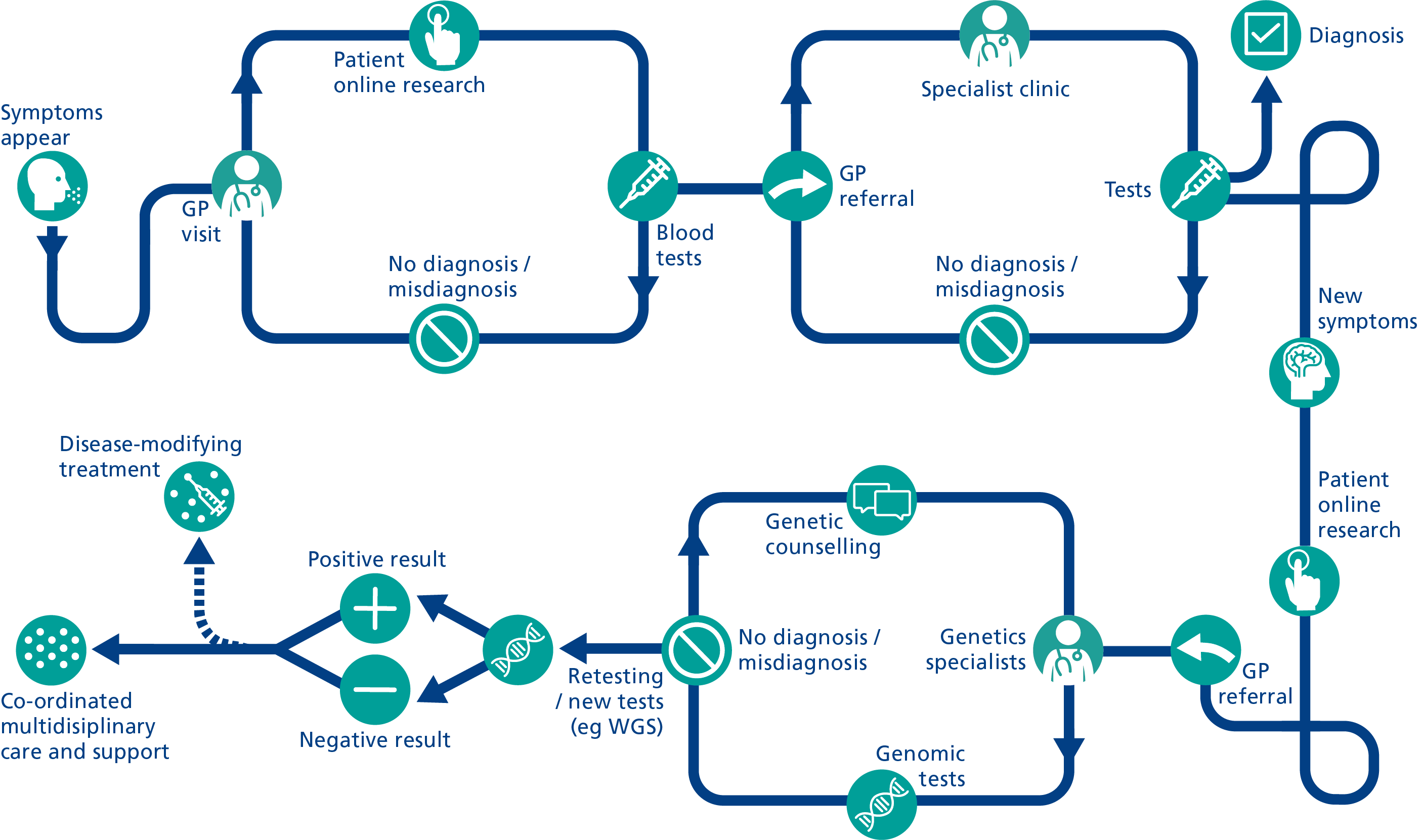
Rare disease patients will often be seen by numerous healthcare professionals across several different specialties, all of whom may offer diverging opinions or diagnoses. This usually involves multiple appointments that are geographically dispersed, often with little communication between services – which can lead to an incorrect diagnosis or even delivery of the wrong treatment. This experience is so common within the rare disease community that it has its own name: the diagnostic odyssey (see figure 1).
Figure 1: The early stages of the diagnostic odyssey. Adapted, with kind permission, from the EURORDIS-led Community Engagement Task Force image ‘Patient Journey through diagnosis’, with input from Medics for Rare Disease.
When a patient has a multisystem condition, the ‘medical ping-pong’ between specialists often means that nobody is looking at the whole picture. For those patients who do receive an accurate diagnosis, many report that they were finally diagnosed when a new doctor listened to their story from beginning to end. Patients may encounter scepticism from multiple healthcare professionals, and many report having to deal with frustrating referral loops (see figure 2). These experiences can result in a patient waiting years for the correct diagnosis and treatment.

Figure 2: The referral loop
It is important to remember that, from the patient’s perspective, receiving a diagnosis is not the only thing that matters: the way in which the diagnosis is obtained and delivered, and the ways in which the patient is supported through the process, are both crucial elements of improving the rare disease patient experience.
The patient experience of the diagnostic odyssey
A person living with an undiagnosed condition will often have no relief from symptoms during their journey to diagnosis. They may also face doubts and dismissal from healthcare professionals. Emotions and challenges experienced can include:
- feelings of isolation, fear and stress;
- deterioration of physical and mental health;
- financial difficulties;
- impacted career and education opportunities; and
- breakdown of personal and/or familial relationships.
In working out how best to support someone living with a rare condition, there is often a process of trial and error. As rare diseases present with so many unknowns, it is important that healthcare professionals across specialties and services work together to deliver the best possible outcome for the patient.
Why do some conditions remain undiagnosed?
Because 80% of rare diseases have a genetic cause, most patients who present with symptoms of a rare condition are diagnosed through genomic testing. Typically, testing will identify a particular variant in a particular gene, which clinicians know to be pathogenic (disease-causing) and linked to a specific condition. However, if a patient is the first person recorded to have a particular genetic variant, even it is suspected to cause their symptoms, their condition will not have been categorised as an existing rare disease.
Alternatively, genomic testing may identify a genetic variant that is not known to cause disease. This is known as a variant of uncertain significance, and because it is not possible to say with certainty whether it causes the patient’s condition, it is not deemed clinically actionable.
Another reason why a condition may go undiagnosed is variation in symptom presentation: sometimes, a patient’s condition presents in a way that is different to most other people with the same condition, meaning that the wrong genes are tested or the wrong type of testing is conducted.
Watch this short video to hear Claudia talk about her son’s rare condition, which currently has no diagnosis.
Receiving a diagnosis
Mixed feelings can arise in the patient and their family when a diagnosis is made. The emotional impact of any diagnosis will depend on whether it has been sought out or is unexpected (that is, the result of an incidental finding from other investigations). When delivering news of a diagnosis, it is important for healthcare professionals to be mindful of the patient’s experience.
The benefits of receiving a diagnosis
For patients, it can be a relief to receive a diagnosis: it provides them with knowledge about their condition, including possible treatment options, and allows for family planning conversations. Healthcare professionals may also feel better equipped to offer coordinated care and condition management, and to seek out research opportunities. While many patients do not wish to be defined by their rare condition, receiving a diagnosis can provide them with the vocabulary they need to explain what they are experiencing, and can help them to feel validated. It may also help them connect with others with the same condition or a similar condition.
Watch this short video to hear Loretta’s story about her long journey to receiving her diagnosis.
The challenges of receiving a diagnosis
On the other hand, receiving a diagnosis can sometimes be scary or frustrating for patients – especially if they are not given adequate information or support afterwards. A 2016 report from Rare Disease UK found that four in five respondents did not receive information about patient support groups from a specialist at the time of diagnosis.
It is also important for clinicians to consider the significance of language when discussing a diagnosis, and to learn about communication techniques when conveying the results of genomic testing. A good place to start is Genetic Alliance’s ‘Good Diagnosis Report’, which provides information about delivering a diagnosis in a way that is accurate, timely, informed, supported, collaborative, coordinated, respectful and acknowledged. A useful framework for delivering bad news can be found on the Accelerate Learning Community website.
How can the diagnostic odyssey be avoided?
It is impossible to be familiar with more than 7,000 rare diseases. However, it is possible to recognise the patterns that suggest that someone may be on a rare disease diagnostic odyssey.
Every healthcare professional can help to reduce the time it takes to get an accurate diagnosis by simply considering that a patient may have a rare disease in the first instance. Despite the rarity of these conditions, every patient should be given care plans, medication reviews, mental health reviews and family planning advice to support them at a time when they need it most.
Resources
For clinicians
- Accelerate Learning Community: SPIKES: A strategy for delivering bad news
- Genetic Alliance UK: Good Diagnosis Report (PDF, 29 pages)
- Genomics England: 100,000 Genomes Project participant stories – Alex (video, two minutes 47 seconds)
- Illumina: Impact of genetic sequencing for rare disease diagnosis (video, one minute 58 seconds)
- Medics4RareDiseases: Available courses
- Medics4RareDiseases: Reducing the diagnostic odyssey (video, 35 minutes 55 seconds)
- Rare 2030: The Rare 2030 recommendations
- Rare Disease UK: The rare reality: An insight into the patient and family experience of rare disease
For patients
- Genomics England: 100,000 Genomes Project participant stories – Alex (video, two minutes 47 seconds)
- SWAN UK