Variant of uncertain significance (VUS)
A variant of uncertain significance is a genomic variant about which there is insufficient data to conclude that it is either benign or pathogenic.
Overview
The variant of uncertain significance (VUS) classification encompasses variants with a wide range of probabilities of pathogenicity, from 10% to 90%.
‘Hot’ VUSs (those that have narrowly missed a ‘likely pathogenic’ classification) are sometimes investigated further to gather evidence which may result in a more definitive classification.
VUS are not considered clinically actionable and cannot be used to alter a patient or family’s management.
What is a VUS?
Genomic variants identified through genomic testing are subject to variant interpretation, to assess their clinical significance. This involves a variety of computer and laboratory techniques, as well as clinical assessment of the patient and family.
Variant interpretation classifies results into five tiers, as set out in the ACMG/AMP guidelines. The possible outcomes, with the probability of pathogenicity for each classification, are:
- Pathogenic (>99%)
- Likely pathogenic (>90%)
- Uncertain significance (10-90%)
- Likely benign (<10%)
- Benign (<0.1%)
If it is not possible to definitively classify a variant as either likely benign/benign (harmless) or likely pathogenic/pathogenic (disease-causing), it is classified as a VUS.
Sub-classification
The VUS classification encompasses variants with a wide range of probabilities of pathogenicity, from 10% to 90%. This group, therefore, includes variants that narrowly missed a ‘likely benign’ classification, as well as those that were just short of being classified as ‘likely pathogenic’.
Sub-classification can be useful, and ranges from ‘ice cold’ to ‘hot’, with a ‘hot’ VUS being one that has narrowly missed a ‘likely pathogenic’ classification.
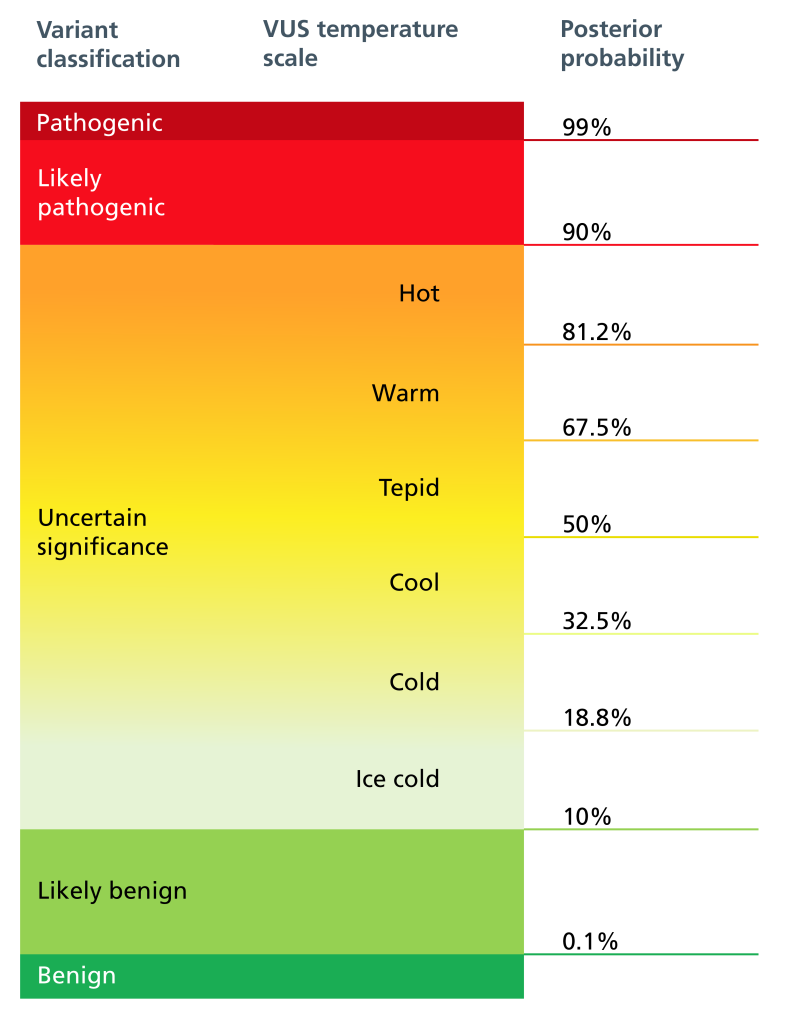
Figure 1: Genomic variant pathogenicity and temperature scale
VUS at the lower end of this range, where further testing would not alter the classification, termed ‘cold’, are unlikely to be disease-causing and are therefore excluded from genomic reports to minimise confusion regarding their relevance.
Clinical laboratories will, however, usually report warm/hot findings, where gathering additional evidence may alter the classification.
Further investigation
Variants that have just missed a likely pathogenic classification due to lack of evidence (so-called ‘hot’ VUSs) often benefit from discussion and further investigation.
These discussions may take place in a genomics MDT; these multi-disciplinary team meetings enable clinicians and clinical scientists to work together to ascertain whether any further evidence can be gathered to aid a more definitive classification for the variant.
The following things may be considered:
- Are there any phenotypic features that could result in the VUS being upgraded?
- Discussion of additional phenotypic detail and/or reviewing photographs with a clinical geneticist in an MDT may result in a hot or warm VUS being upgraded to likely pathogenic or pathogenic.
- Would testing of any other family members help to gather more information about the variant?
- Testing of parents may be requested, if not already done, to ascertain whether a variant in an affected child has arisen de novo or been inherited from a parent. If the variant was inherited from a healthy parent it makes it less likely to be the cause of the child’s difficulties.
- Testing in other family members may give segregation data, allowing a clearer picture of whether the variant in question is present in other family members, and how or if they are affected clinically, which may result in a more definitive classification of the variant.
- Note, when interpreting familial data, the possibility of reduced penetrance must be kept in mind.
- Are there any additional investigations that could help?
- MDT discussions can help identify when additional investigations, such as biochemical testing or additional imaging, would be beneficial to variant interpretation. Sometimes specialist genetic tests, such as functional (mRNA) studies, which can show whether a variant affects splicing, may be suggested.
In this film, Dr Asma Hamad discusses the different outcomes that can arise from testing and the further investigations that can be required.
Does identifying a VUS change a patient's management?
VUS are not considered clinically actionable and cannot be used to alter a patient or family’s clinical management.
The consequences of a misdiagnosis due to variant misclassification can be harmful, not only to the individual in whom the pathogenic variant is detected, but also to family members whose clinical management may be affected because of what is known as cascade testing (genomic investigations resulting from a diagnosis in a relative).
For this reason, only ‘pathogenic’ and ‘likely pathogenic’ variants can be used in clinical decision-making — not VUS. In the context of a VUS, clinical management decisions (such as screening) are made on the basis of personal and family history alone, and cascade testing should not be offered to family members.
Note: In the context of a VUS, testing may be done within the family to gather segregation data to aid a more definitive classification, but not cascade testing to determine clinical management for the family.
What if a classification changes?
In some instances, VUS are subsequently up- or downgraded further down the line, with the accrual of more population-level and diagnostic data. This change may be reported in the scientific or medical literature.
Note, however, that laboratories don’t currently have the capacity or resources to monitor the status of VUS to see if the classification changes over time; this should be discussed with patients, or parents, who should be advised to re-consult in a few years’ time in case of any update.
Key messages
- A variant of uncertain significance (VUS) describes a genomic variant about which there is insufficient data to conclude that it is either benign or pathogenic.
- VUS that have just missed a likely pathogenic classification (so-called ‘hot’ VUS) may benefit from further investigation, to gather evidence for a more definitive classification.
- VUS are not considered clinically actionable and cannot be used to alter a patient or family’s clinical management.
Resources
For clinicians
- NHS England Genomics Education Programme (GEP): Genomics in the NHS: A Clinician’s Guide to Genomic Testing in Rare Disease
- NHS England GEP: Interpreting results: Beware the amplification of error (film, 4 min)
References:
- Richards S, Aziz N, Bale S and others. ‘Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology‘. Genetics in Medicine 2015: volume 17, issue 5, pages 405–424. DOI: 10.1038/gim.2015.30
- Joynt A, Axford M, Chad L and others. ‘Understanding genetic variants of uncertain significance‘. Paediatric Child Health 2021: volume 17, issue 1, pages 10–11. DOI: 10.1093/pch/pxab07